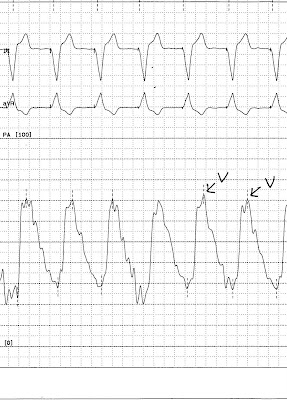
Picture Diagnosis

Answer: Long linear bands of atelectasis (Fleischner lines)
This is a normal CXR done in an acutely hypoxic patient with PE (pulmonary Embolism). Usually missed are these minor long linear bands of atelectasis called Fleischner lines - may be associated with unilateral or bilateral PE. Unilateral or bilateral pleural effusions may also be present.